Did the ADA get it Wrong with Hyperbaric Medicine?
- Dick Clarke, CHT-Admin

- Jun 10, 2020
- 4 min read
Updated: Jun 12, 2020

The American Diabetes Association has long discounted the value of HBO therapy for diabetic foot ulcers, and their “Standards of Medical Care in Diabetes-2020” is no exception.
This influential practice guideline placed emphasis on one particular study (Fedorko L, et al. 2016) that, in my view, represents the single most scientifically deficient of any published hyperbaric efficacy research. The ADA thought otherwise, “A well-conducted randomized controlled study performed on 103 patients found that HBOT did not reduce the indication for amputation or facilitate wound healing compared to comprehensive care”. ‘Indication’ is my emphasis and more on that soon.
One might be inclined to excuse the busy clinician for skimming over new publications, particularly when the subject matter doesn’t represent their primary specialty/practice; a wound care specialist who also covers HBO, for example. One cannot be as forgiving for those responsible for development of clinical practice guidelines. This level of responsibility demands more in-depth analysis than a simple reading of a paper’s Abstract and acceptance of its Conclusions.
Major Fedorko RCT deficiencies
Perhaps the most startling of several study design and execution flaws was the manner in which the primary outcome measure, freedom from amputation, was determined. At 12 weeks post-hyperbaric treatment/sham chamber exposure, a designated vascular surgeon was to evaluate study subjects. He was required to make a yes/no determination, based not on clinical experience, but upon four factors as to whether patients had an indication for amputation. If any of these four was 'yes', he was required to adjudicate to amputation. Even more disconcerting, wound photos had been substituted for patient visits in a majority of instances. This non-validated research method served as the sole source from which to adjudicate most patients, representing both study protocol and patient informed consent violations.
If there was persistent localized deep infection, (for which standard of care might dictate hospitalization, pathogen identification and antibiotics) adjudication to amputation was mandated. Likewise, any open wound in these patients, no matter the degree, ‘represented risk for systemic infection’, so adjudication to amputation was required. Inability to bear weight faced the same adjudication decision, rather than consideration of an off-loading strategy. Finally, pain causing significant disability (I cannot figure out how this was diagnosed from a wound photo) met the same adjudication fate. Given the protocol’s yes/no decision mandates, the surgeon’s administrative assistant may have been an equally effective assessor.
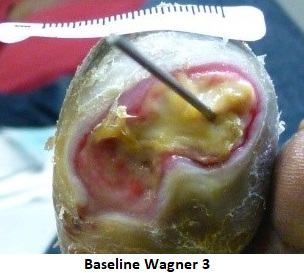
Here are two examples of this somewhat bizarre assessment process:
*Linden R, 2013
Not surprisingly, this form of assessment failed miserably. Of 17 patients adjudicated to amputation, only three underwent amputation, representing an error rate of 82%. (Linden R, 2103) A true rate that would have distinguished between virtual and actual amputations did not feature in the Fedorko et al. publication because the ‘per protocol’ requirement for a 52-week follow-up did not occur. In fact no data beyond the 16 week follow-up, including the protocol mandated 30 week follow-up was reported by Fedorko et al.
Another glaring shortcoming was a failure of any reference to the fact that the study included a crossover arm. Sham patients eventually had the opportunity to cross over to HBO, and most did. Their subsequent benefit from active therapy likewise went unreported. The ethics committee approved protocol also indicated routine tissue oximetry screening and other vascular assessments, none of which took place.
Reference to the International Working Group on the Diabetic Foot
It is also worth commenting on a marked disparity between the ADA’s interpretation of the 2016 IWGDF guidance document and what was written. The ADA incorrectly suggested that this group ‘…concluded that analysis of the evidence continues to present methodological challenges as randomized controlled trials remain few, with a majority being poor quality”. Contrast this with the IWGDF recommendation to ‘Consider the use of systemic hyperbaric oxygen therapy, even though further blinded and randomized trials are required to confirm cost-effectiveness, as well as to identify the population most likely to benefit.’ The IWGDF went on to add that in their systematic review ‘…we reported two RCT’s of methodologically good quality on systemic hyperbaric oxygen therapy. (Abidia A, et al. 2003; Londahl M, et al. 2010). The larger (Londahl) study, which included patients with and without (severe) peripheral arterial disease, demonstrated significantly improved outcome in the intervention group, who were more likely to heal within 12 months.’ This certainly offers a more encouraging viewport than the one the ADA had appeared to ‘titrate to effect’ The IWGDF document rightly referenced a large effectiveness study (Margolis D, et al. 2013) that failed to demonstrate benefit, due in large part to a flawed patient selection process.
A majority of diabetic foot ulcers are likely to heal absent HBO therapy. There is little argument, then, for improved efficacy data to better define at what point and in whom HBO therapy might prove helpful. There is certainly room to better define the hyperbaric dosing protocol. However, these shortcomings should not distract from observations that in carefully selected patients, this treatment modality has improved rates of healing and reduced the incidence of major amputations.
References available upon request
















I never expected an online platform to be this fun until I tried Laser Book 247. It brings all the thrills of live sports into a simple, engaging setup. You’ll love how easily it runs and how many exciting features it offers.